Many people think of blood sugar as something that only people with diabetes need to think about, but the truth is that everyone can benefit from knowing their blood glucose levels.
Diabetes is often called a silent disease because there aren’t many symptoms, especially in the beginning. You can have high blood sugar levels or insulin resistance for years before developing diabetes. Blood sugar dysregulation and higher insulin levels can make it harder to lose weight, impact energy levels, and even affect mood.
This article will help you understand normal blood sugar ranges, why glucose matters for your health, and what steps you can take to stabilize your blood sugar.
{{mid-cta}}
What Is Blood Sugar?
Glucose, or blood sugar, is the sugar found in your blood and serves as your body’s primary energy source. When your glucose is elevated, insulin gets released by the pancreas to move the glucose into cells for immediate energy. Glucose that isn’t used gets stored for later, often as fat.
Many foods that you eat can increase glucose levels in your body. In an ideal state, your body’s complex hormonal responses will keep glucose in a healthy range. However, excess fat, insulin resistance, pre-diabetes, and other factors can cause higher, longer glucose spikes.
Knowing what happens when blood sugar is out of range and why it happens helps us better understand what's considered an optimal blood sugar range.
Under healthy conditions, the pancreas releases insulin when glucose levels are high. Insulin signals your body to absorb the glucose until your levels drop back into range.
People with type 1 diabetes or type 2 diabetes may not make enough insulin, or the cells don’t respond to insulin as they should. As a result, blood sugar levels remain high for too long and can damage nerves and blood vessels, which can lead to serious health issues like heart disease and kidney disease.
What Is Hypoglycemia?
Hypoglycemia occurs when an individual has low blood sugar or when the glucose in your blood drops below 70 milligrams per deciliter (mg/dL).1 Some people will have a different range of normal (i.e., a lower normal range). Severe hypoglycemia happens when your blood glucose drops so low that you cannot do anything for yourself, and you should seek treatment immediately.
Low blood sugar rarely results from not eating enough or burning fuel during a long cardio workout. One of the most common causes of true hypoglycemia is accidental low blood sugar from medications that treat diabetes, like insulin or sulfonylureas. People who have had bariatric surgeries can also experience hypoglycemia events.
Other causes of hypoglycemia include critical illness, malnutrition, and a variety of rare conditions like insulin-secreting tumors and adrenal insufficiency (when your adrenal glands do not produce enough steroids like cortisol). These are serious conditions and should be closely monitored by a healthcare provider.
What Is Hyperglycemia?
On the other end of the spectrum, hyperglycemia (high blood glucose) occurs when too much sugar is in your blood (a fasting glucose of more than 125 mg/dl for those without diabetes).2
Chronic hyperglycemia over a consistent period is a symptom of diabetes. Hyperglycemia can lead to the following diabetes complications and risk factors:3
- Diabetic retinopathy: Abnormal blood vessels on the retina that can cause vision impairment.
- Nephropathy: Impaired kidney function that can lead to kidney disease.
- Neuropathy: Nerve damage.
- Coronary artery disease: Plaque buildup in the arteries that could eventually lead to a heart attack.
- Cerebrovascular Disease: Impairs blood flow to the brain, which could lead to stroke.
- Depression.
- Diabetic ketoacidosis (DKA): A medical emergency that requires immediate attention and could lead to organ damage, brain swelling, muscle weakness, and a heart attack or heart failure.
What Affects Blood Glucose Levels

Several factors influence your blood glucose levels. Some are modifiable (meaning you can make positive lifestyle changes to help optimize blood sugar), while others are non-modifiable. By understanding all of these factors, you can take steps ahead of time to support your metabolic health.
Age
Age is a risk factor for developing type 2 diabetes. Blood sugar rises as you age, possibly related to insulin resistance or the pancreas making less insulin.4 Women are also at increased risk for becoming insulin-resistant during perimenopause and menopause, which is linked to declining estrogen levels.5
Foods You Consume and Meal Timing
Your food choices are the most significant factor influencing your blood glucose levels. A healthy diet can reduce postprandial blood glucose spikes (after meals) and improve insulin sensitivity.
Our bodies also have natural circadian rhythms determined by an internal biological clock that responds to light and darkness in the environment. Circadian rhythms affect everything from hormones to body temperature to metabolism.
When these rhythms are disrupted, they can lead to metabolic issues like insulin resistance. One study found that insulin sensitivity (or how responsive the cells are to insulin) was 54 percent higher before noon than at midnight.6
Another study found that when men with pre-diabetes ate earlier in the day (before 3 p.m.), metabolic markers like insulin sensitivity, blood pressure, and oxidative stress all improved compared to a regular 12-hour eating window.7
To help reduce spikes, try pairing carbohydrates with proteins and healthy fats. Minimize highly processed foods, added sugars, high-glycemic-index foods, and excessive alcohol consumption. Instead, stay hydrated and focus on healthy fats, high-fiber carbs, whole grains, and protein in your meals.
Health Conditions and Medication
Health conditions, such as diabetes and obesity, can directly affect your body’s ability to produce and use insulin. Since insulin is critical in regulating glucose levels, the type of diabetes you may be living with or other medical conditions can impact your blood sugar levels.
Medications can also influence glucose levels. Some are explicitly designed to lower blood glucose, but others, like steroids, can increase it. Make sure you discuss any medications with your care team.
Exercise and Sleep
Daily movement is linked to better blood sugar by supporting weight management, insulin sensitivity, and blood sugar control.
However, there is such a thing as “too much” when it comes to exercise, so make sure you are giving yourself proper rest and talk to your doctor, personal trainer, or other health and wellness practitioner about what is right for you.
Sleep is just as important as movement. A lot happens in your body while you’re sleeping. Aside from dreaming, memory formation, muscle repair, and other functions, your body actively manages glucose during slumber. Some research ties sleep disruptions with poor glucose control.8
Stress
Epinephrine, cortisol, growth hormone, and glucagon—the stress hormones—work together to release glucose into your bloodstream, among other changes. These changes help you stay sharp and focused and give you extra energy.
Your adrenal glands release adrenaline and cortisol to encourage your liver to produce more glucose for quick energy during stressful situations. Growth hormone, secreted from the pituitary gland in your brain, also halts the effects of insulin.9
This sophisticated system works well when dealing with a real threat or challenge, but blood sugar levels can remain high if you’re constantly stressed out.
To counteract high glucose levels, your pancreas releases insulin to help your body use or store excess glucose. Over time, chronically elevated insulin levels may lead to insulin resistance, where you need even more insulin to help the cells absorb the extra glucose in the blood. Insulin resistance may lead to type 2 diabetes and other chronic illnesses.
Does a Blood Sugar Spike Mean You Have Diabetes?
Occasional high spikes don’t mean you have diabetes. It’s normal for your blood sugar to go up after eating a meal high in carbohydrates or even due to lifestyle habits and events. Besides food, stress, lack of sleep, age, menstrual cycle, physical activity, and even being sick can affect your blood sugar.
What affects one person's blood sugar may also affect yours differently, so monitoring the overall trend of your blood sugar gives you the most insight into your overall health.
However, while infrequent spikes aren't a problem, if they happen more regularly, it’s time to take a closer look.
What Are Normal Glucose Levels for People Without Diabetes?
Normal blood sugar levels for people without diabetes are as follows:10
- Fasting: 70-99mg/dl (100-125mg/dl for those with pre-diabetes)
- Post-meal: Less than 140mg/dl at 2 hours post-meal
- A1C: 4-5.6%
Most blood sugar charts show recommended levels as a range, allowing for individual differences. Some people may find their blood sugar is much lower while others hover a bit higher, but the ranges above are considered diagnostic cut-offs by medical professionals.
It’s also helpful to note that most blood sugar guidelines are used as standards of medical care in diabetes to differentiate between a diabetes diagnosis and “normal” blood sugar. Still, optimal blood sugar for healthy adults may be even lower.
For example, if your fasting blood sugar is always 99mg/dl, while this is technically normal, it’s only a small difference between prediabetes, so supporting stable blood sugar is especially important.
<div class="pro-tip"><strong>Learn More: </strong><a href=normal-blood-sugar-levels-chart>Normal Blood Sugar Levels by Age: Charts Explained</a>.</div>
What Are Normal Glucose Levels for People Living With Diabetes?
People living with diabetes will often have higher blood sugar targets or “acceptable” ranges than those without the condition. However, these levels can also vary individually depending on a person’s treatment goals.
According to the American Diabetes Association (ADA), target blood sugar levels for non-pregnant people with diabetes are as follows:11
- A1C: Less than 7%
- Pre-meal Glucose: 80-130mg/dL
- Post-meal Glucose: Less than 180mg/dL one to two hours after the beginning of a meal
Blood Sugar Metrics You Should Check

There are multiple types of blood sugar metrics, some more common than others. Each one gives a slightly different picture of your glucose levels. Here are blood sugar test options:12
Fasting Glucose
Fasting glucose measures the blood sugar levels after fasting for at least 8 hours. Anything below 100mg/dl is considered normal. Fasting blood sugar levels above 100 indicate pre-diabetes and anything above 126mg/dl is considered diabetes.2
Pre-meal Baseline Glucose
This is your blood sugar level before eating. It may be fasting, but it could also be between meals. The range varies for people without diabetes, but ideally, your blood sugar will drop to 70 to 100mg/dl for healthy adults (assuming you haven’t eaten recently).
Post-meal Glucose
Also called postprandial blood glucose, this reading will tell you your blood sugar one to two hours after a meal. As noted above, for people without diabetes, blood sugar should drop below 140mg/dl by two hours after a meal. Some will be much lower, especially if the meal is low in carbohydrates.
A1C Test
Hemoglobin A1C (or HbA1c) is the standard metric for diagnosing diabetes or assessing how well-managed blood sugar is for people with and without diabetes. This test provides your average blood sugar levels over the past three months.
Anything under 5.7% is considered normal, 5.7 to 6.4 suggests prediabetes, while over 6.5% is regarded as a diagnosis of diabetes.2
Time-In-Range
Time in range tells you the percentage of time you have spent within a target range. This range can vary between individuals and can be helpful for people without diabetes who are trying to optimize metabolic health. It’s also used in diabetes care to assess how well someone with diabetes meets their blood sugar targets.
How to Test Your Blood Sugar Levels
The above metrics can be obtained in several ways. Some can be done at a lab, while others are taken at home.
Blood glucose is measured in milligrams per deciliter (mg/dL), but you may also see test results listed in mmol measurements. Always discuss test results with a healthcare professional if you have questions.
Lab Testing
Labs provide blood tests and typically require a doctor’s order. This is often done during an annual check-up or for routine blood work. Your lab results usually include blood samples for A1C and fasting blood glucose levels. Sometimes, a lab will also take a plasma glucose test, which doesn't require fasting (anything below 200mg/dl is considered normal for this test.
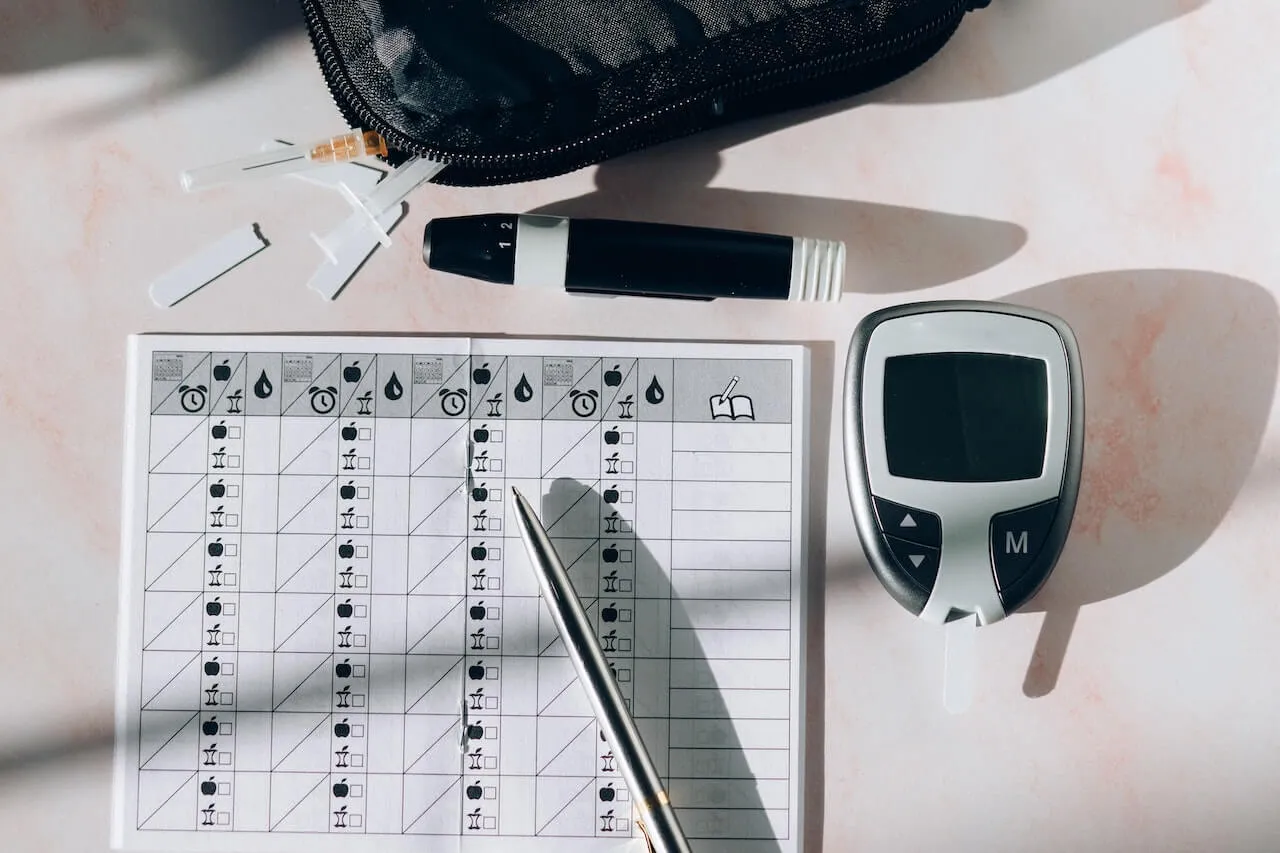
Home Glucometer
A glucometer is a handheld device that measures blood sugar. You prick your finger and place a drop of blood on a test strip, which gives you an immediate reading of your current blood sugar level. Some models have additional features like tracking readings over time or connecting to a smartphone app for easier monitoring. People with diabetes most commonly use these to manage their blood sugar levels daily.
OGTT
Often used in pregnancy to assess for gestational diabetes, the oral glucose tolerance test (OGTT) requires drinking a specific amount of glucose and testing glucose at one, two, and sometimes 3 hours after. Greater than or equal to 200mg/dL two hours of ingesting glucose is considered a diabetes diagnosis.2
Continuous Glucose Monitors
While not diagnostic, continuous glucose monitors (CGMs) measure blood glucose levels in real-time. Unlike other at-home tests that use a glucometer to take a finger prick, a CGM sensor is painlessly implanted into your arm or upper stomach and can be worn continuously for 10-14 days.
A small filament on the backside of the CGM sensor sits just below the skin. The filament tracks and records the glucose levels in the interstitial fluid (a fluid that fills the spaces between your cells).
The sensor takes a glucose reading every 5-15 minutes, even while you sleep. The data is sent via Bluetooth to your smartphone, where you can review trends or any noteworthy changes in blood sugar levels.
Using a CGM with Signos: Real-Time Data, Backed by AI
Signos pairs a real-time glucose biosensor with AI trained on tens of millions of data points to deliver personalized, science-backed guidance. See exactly how your body responds, and take action.
Learn how it works. Ready to get started? Join now.
Topics discussed in this article:
References
- National Institute of Diabetes and Digestive and Kidney Diseases. “Low Blood Glucose (Hypoglycemia) | NIDDK.” Retrieved from: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/low-blood-glucose-hypoglycemia.
- American Diabetes Association. (n.d.). ”Diabetes Diagnosis & Tests”. Retrieved from: https://diabetes.org/about-diabetes/diagnosis.
- Medline Plus. (n.d.). Retrieved from: https://medlineplus.gov/ency/patientinstructions/000327.htm
- Chia, C. W., Egan, J. M., & Ferrucci, L. (2018). Age-Related Changes in Glucose Metabolism, Hyperglycemia, and Cardiovascular Risk. Circulation research, 123(7), 886–904. https://doi.org/10.1161/CIRCRESAHA.118.312806
- De Paoli, M., Zakharia, A., & Werstuck, G. H. (2021). The Role of Estrogen in Insulin Resistance: A Review of Clinical and Preclinical Data. The American journal of pathology, 191(9), 1490–1498. https://doi.org/10.1016/j.ajpath.2021.05.011
- Carrasco-Benso, M. P., Rivero-Gutierrez, B., Lopez-Minguez, J., Anzola, A., Diez-Noguera, A., Madrid, J. A., Lujan, J. A., Martínez-Augustin, O., Scheer, F. A., & Garaulet, M. (2016). Human adipose tissue expresses intrinsic circadian rhythm in insulin sensitivity. FASEB journal : official publication of the Federation of American Societies for Experimental Biology, 30(9), 3117–3123. https://doi.org/10.1096/fj.201600269RR
- Sutton, E. F., Beyl, R., Early, K. S., Cefalu, W. T., Ravussin, E., & Peterson, C. M. (2018). Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell metabolism, 27(6), 1212–1221.e3. https://doi.org/10.1016/j.cmet.2018.04.010
- Mesarwi, O., Polak, J., Jun, J., & Polotsky, V. Y. (2013). Sleep disorders and the development of insulin resistance and obesity. Endocrinology and metabolism clinics of North America, 42(3), 617–634. https://doi.org/10.1016/j.ecl.2013.05.001
- Kim, S. H., & Park, M. J. (2017). Effects of growth hormone on glucose metabolism and insulin resistance in human. Annals of pediatric endocrinology & metabolism, 22(3), 145–152. https://doi.org/10.6065/apem.2017.22.3.145
- American Diabetes Association. (n.d.). ”Diabetes Diagnosis & Tests”. Retrieved from: https://diabetes.org/about-diabetes/diagnosis.
- “The Big Picture: Checking Your Blood Glucose | ADA.” (n.d.) Retrieved from: https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/checking-your-blood-sugar
- National Institute of Diabetes and Digestive and Kidney Diseases. “Diabetes Tests & Diagnosis | NIDDK.” Accessed May 26, 2022. https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis.




.svg)









.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
